Altering the blood type of lungs raises potential for universal organs for transplants


It was 4 a.m. on a moist evening in St. Catharines, Ontario, and Elizabeth Ostrander couldn’t breathe. Continual obstructive pulmonary illness, difficult by pneumonia, was suffocating her, medical doctors instructed her that day in 2016. If she hadn’t gotten to the hospital when she did, she would have died, Ostrander remembers them saying. She was in her early 50s.
She would spend the subsequent 5 years hooked to an oxygen tank, cords tangling round her in her sleep. The incurable illness worsened till she had simply 25% of her lung capability left. It was so troublesome to breathe that she might barely lug groceries from her automotive to her kitchen, a lot much less be the “avid camper” she was earlier than. She needed to cease working, and was positioned on the lung transplant ready record. When the Covid-19 pandemic hit, she thought, “I’m by no means going to get my lungs.”
She lastly did, on Nov. 13, 2021, nevertheless it took almost two years of ready and three false alarms.
commercial
Ostrander was in the identical bind as many individuals awaiting transplants. Her blood kind, B constructive, wasn’t a match for a lot of donor organs, and a mismatched transplant could be catastrophic and deadly. However new analysis suggests this barrier might disappear if donor organs have been handled with particular enzymes that make them appropriate with recipients of any blood kind.
“This analysis can be a game-changer in organ transplantation,” stated Aizhou Wang, the lead creator of a paper published Wednesday in Science Translational Medicine. “For contemporary transplant drugs, matching is all the time a part of the standards if you find yourself looking for the appropriate organ for a recipient.”
commercial
And blood kind is all the time one of many first concerns that limits what organs a affected person can obtain, she stated. A hospital might have a donor organ, and it’s wholesome, it’s the correct dimension for the affected person and geographically close by, but when it’s an incompatible blood kind, the recipient’s immune response would destroy the organ throughout the first 48 hours.
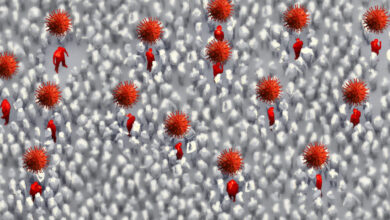
This mismatch, decided by an array of immune system foot troopers on the floor of purple blood cells and blood vessels, is an issue throughout the three principal blood sorts: A, B and O. For sufferers with type-O blood, who can solely obtain an organ from one other O donor, their threat of dying whereas ready for a transplant is 20% larger than for these with different blood sorts. Black and Latino individuals are extra doubtless than whites to have type-O blood.
Within the fall of 2018, researcher Aizhou Wang sat with Marcelo Cypel, her supervisor and a lung transplant specialist on the Toronto Normal Hospital Analysis Institute. They have been looking for a venture for Wang to focus her postdoctoral analysis on, and a nook of the scientific world was abuzz with enzymes. Extra particularly, individuals have been speaking about work led by Stephen Withers on the College of British Columbia. His group had found a brand new pair of enzymes within the human intestine that might change blood kind from A to O — and accomplish that extraordinarily effectively, far more effectively than every other, comparable enzymes that had been beforehand discovered.
The enzymes go round like a pointy pair of scissors, neatly shearing off a sugar known as GalNAc from A-antigens that line the floor of purple blood cells, in addition to cells within the lungs, till they resemble O blood kind. That transformation, Withers realized, might neutralize no matter battle may come up when warring antigens and antibodies meet throughout a mismatched organ transplant. In Cypel and Wang, Withers discovered researchers keen to discover that speculation.
Their analysis reveals proof-of-concept: Lungs from a type-A donor might be handled with the enzymes for a number of hours and emerge with the mobile look of getting O blood kind. And, the handled lungs weren’t broken once they got here into contact with O blood plasma throughout a transplant simulation. “Like a camouflage,” Cypel stated. Antibodies “received’t acknowledge the cells anymore as being a special blood kind.”
About 85% of individuals have both A or O blood kind, so engineering organ compatibility between the teams would vastly increase transplant choices for these sufferers, Cypel stated. If medical doctors might take away ABO blood kind matching from the equation fully, that might take away a serious logistical hurdle and get organs to sufferers in want extra shortly.
“It has the potential – and I’d underline ‘potential’ – to increase the donor pool in significant methods. And we’ve got to consider any method that we will do this, given there’s nonetheless important mortality on the lung transplant ready record,” stated David Weill, former director of the lung transplant program at Stanford College.
Regardless of a marked improve in organ donations during the last decade, the demand for lung transplants is commonly unmet, in line with annual reports from the Organ Procurement and Transplantation Community. Greater than 20% of sufferers on the waitlist for donor lungs wait greater than a yr.
Yearly, “tons of of sufferers die ready for a lung transplant on account of lack of availability of appropriate organs,” stated Nirmal Sharma, medical director of the Lung Transplantation Program at Brigham and Ladies’s Hospital.
A thoracic surgeon, Cypel was one of many researchers who developed ex vivo lung perfusion, a way of preserving lungs at physique temperature in an incubator that mimics the atmosphere of the human physique. EVLP has additionally been discovered to be an efficient method of treating much less wholesome lungs and testing how they could carry out within the human physique. After making an attempt the enzymes on purple blood cells and human aortae, Cypel’s multidisciplinary Canadian analysis group used EVLP to deal with human lungs, after which to show them to O blood plasma. It was a intelligent workaround that got here out of necessity. The researchers couldn’t take the standard route – from easy-to-control small animal (rodent) fashions, to giant animals after which people — as a result of there isn’t any comparable slate of blood sorts in animals.
“I simply had by no means considered utilizing the know-how of those units on this method. In different phrases, I knew all in regards to the type of therapy you are able to do to the organs whereas they’re on the units. I didn’t know we might change the ABO compatibility,” stated Weill, who serves on the board of administrators of TransMedics, creator of a competing organ storage machine.
Cypel is a founder and shareholder of Traferox Applied sciences, which develops different lung storage strategies, together with an EVLP machine. He’s additionally a marketing consultant for Lung Bioengineering, and is looking for a patent for using these sugar-cutting enzymes to vary blood sorts throughout human organs.
The research’s key limitations stem from the truth that handled lungs weren’t implanted in an actual particular person, a number of lung transplant specialists instructed STAT. Operating O blood plasma by means of EVLP can set off a comparable interplay to what would occur within the human physique. However the physique’s immune system is much extra advanced in actual life, and will current some extra challenges.
“It’s nonetheless plasma in isolation. It’s not linked to an precise recipient that has an energetic bone marrow, might have energetic manufacturing of antibodies as a result of T cells and B cells might get activated,” stated Matthew Bacchetta, chair of Vanderbilt College Medical Middle’s Division of Thoracic Surgical procedure.
The subsequent step will probably be testing this organ therapy towards the complete arsenal of instruments a human physique makes use of to destroy the unfamiliar. Plus, the enzymatic haircut isn’t everlasting; antigens, like hair, reappear on cell surfaces in some unspecified time in the future, elevating questions on whether or not the physique might have a adverse response to a mismatched transplant someday after the preliminary 24-hour window post-transplant. Wang, the lead creator, agrees extra analysis is required.
“We do acknowledge we’re eradicating simply the antigen, not the equipment within the physique that makes these antigens,” stated Wang, the paper’s lead creator. “So, over time, we do count on that they develop again step by step. However how briskly? We’re presently making an attempt to review that.”
For individuals like Ostrander, who waited two years for brand new lungs, common organs would make an enormous distinction – giving them again years of their life. “It might’ve modified my entire life,” she stated. “I’d’ve been capable of do extra again then as an alternative of being so restricted.”